Physician-Assisted Suicide among Terminally Ill Patients in the United States
Suicide has been a part of society and has lasting effects on many individuals. It is sometimes supported, but usually condemned. Some people argue that we have a right to die, as an extension on our rights of freedom of speech and freedom of thought. Globally suicide is already the highest in people older than 70. Euthanasia and physician-assisted suicide have become pressing public issues that are not typically discussed, even though it affects the lives and families of many. There are many questions that are raised without answers, such as who should be eligible for physician assisted suicide? Doctors are supposed to save lives. But what if no matter of medical intervention can help change someone’s imminent death? Should doctors then be allowed to help patients die on their own terms? If you allow physician assisted suicide, how close are we to condoning mass physician assisted suicide – what is now known as the Holocaust? Is this a “slippery slope”?
According to the Hippocratic Oath, assisted suicide would be outside of a physician’s professional responsibilities (Jr., W. C. S. ,2018). The five principles of bioethics include autonomy, justice, beneficence, non-maleficence, and fidelity and are each said to be absolute truths in and of themselves. However, beneficence, the prevention of harm or the doing of good, conflicts with respect for autonomy when one considers assisted suicide.
When interviewing Bonnie Hafeman M.D., a family physician with a subspecialty in Hospice and Palliative Care, who has worked in Hospice for 23 years, she said “I think that physician assisted suicide is totally unnecessary because people are given all of the tools they need to control their own death. The easiest way to do so is just to not eat and drink. This is a relatively painless death that takes about a week. And it is natural.”
She states that “It is immoral to involve another human being in your own death because that is really between you and God. I think that when you do physician assisted suicide it is just a publicity stunt.”
I think that this has to do with how they present themselves and how they talk to others. It makes me wonder what kind of relationship they have with their physician. Physicians should be there to give advice and to help plan out where they want to go with their lives, but I don’t think it is right to have another person be responsible for their death. The increase in this event, and the legalization and acceptance of the physician assisted suicide may lead to the undesirable action which is involuntary euthanasia. Once one becomes common practice, society becomes used to something become a norm and it expand it until it reaches a nonlogical position. Once we allow voluntary euthanasia, we may fail to make the distinction and make the morally unacceptable use to use involuntary euthanasia.
Dr. Hafeman goes on to say, “The most commonly cited need for assisted suicide is the condition ALS where your body loses muscle function so you cannot swallow or move so you may end up being locked where you can still see and hear people, but not talk or interact with them. Those same people are also advised to have gastric tubes placed to feed them. If they weren’t being fed artificially they would die naturally by dehydration without ever being locked in. A person should have access to terminal pain control, and how they use this is often beyond the control of the physician who prescribed it. If a person does not have access to pain control the answer is not physician assisted suicide, it is giving the person adequate pain control. Yes, this might hasten a patient’s death. However, it is a balance between intention to commit suicide and a patient’s right to have pain controlled.”
Even though one may wish to alleviate suffering, assisting with death to end the suffering violates the principle of beneficence even though the individual may in autonomy, request death.
In many states, physician assisted suicide (PAS) has been deemed as a socially acceptable way to end a life if there is extreme suffering. As you can see in the figure below, today, it is legal in 10 jurisdictions as of January 2020, with Oregon being the first when they enacted their Dignity Act in 1997.
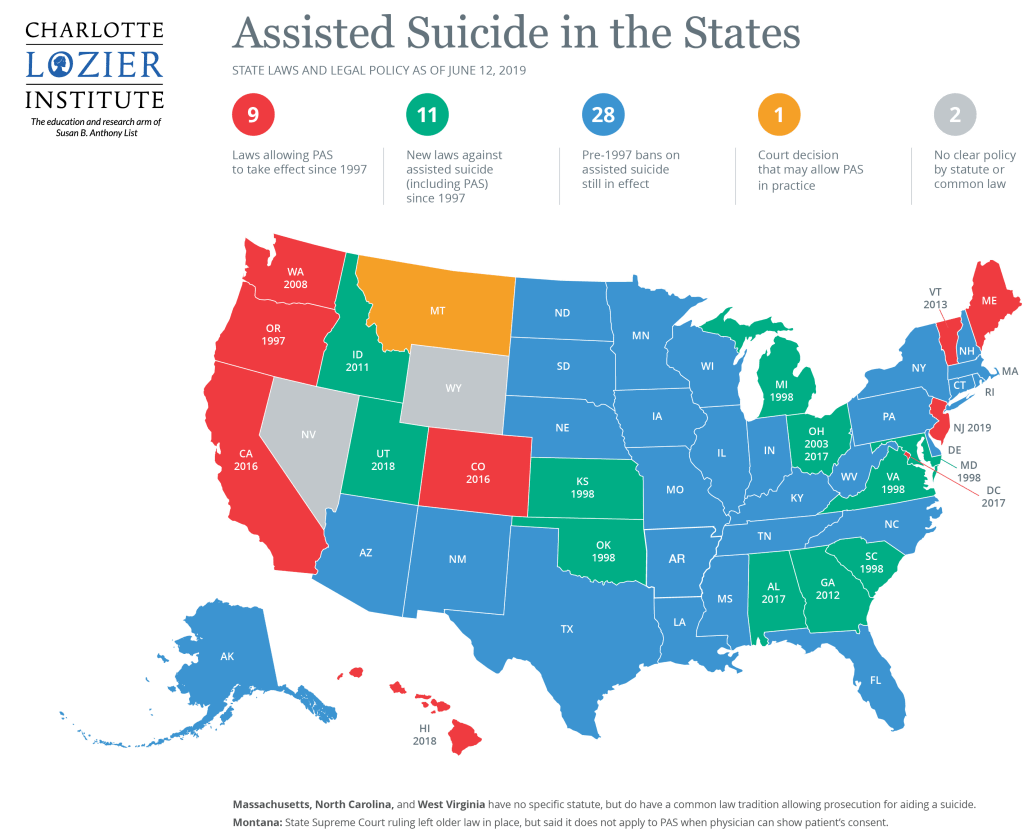
Charlotte Lozier Institute. (n.d.). Map: Assisted Suicide in the States. Retrieved from https://lozierinstitute.org/map-assisted-suicide-in-the-states/
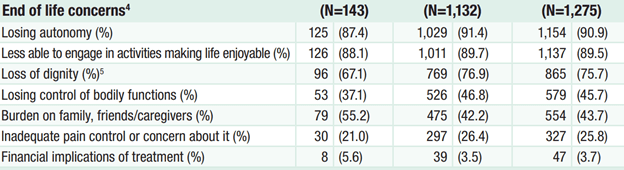
In the figure shown below, you can see that in Oregon, there has been an increase in physician assisted suicides and an even higher increase in requests since it became legal in 1997. These numbers are rising. This act is done by ingesting a lethal medicine dose prescribed by them after the request. The Oregon Death with Dignity act 2017 Data Summary shows that most patients request that request assisted suicide at 88.1% is because they cannot participate in activities making life enjoyable. 87.4% choose to over lose autonomy and 61.7% choose to because of dignity. They give validating reasons for why they choose to go on with PAS. This can all be seen in the data table shown below.
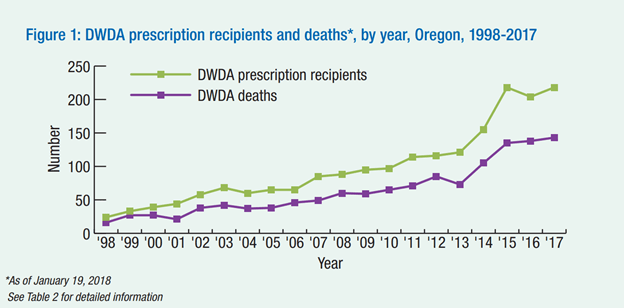
Physician Assisted Suicide. (n.d.). Retrieved from https://illinoisrighttolife.org/physician-assisted-suicide/
As of right now, we are comfortable to allow PAS for people who are terminally ill and near the end of their life, but so far we have dragged our feet when it comes to expanding to those who can gain access to PAS in the United States.
In a survey by Dr. Emanuel done in 2002, he looks at the attitudes of the American publics, of physicians, and of patients. He found that in all three of the survey categories that people who were reported as religious were more likely to be opposed to euthanasia or PAS. This may have to do with the belief in life after death and that the time of suffering or death is a time of awareness or connection with God. It’s not the pain itself that’s an issue, but about the connection with God. African Americans and older individuals are also more opposed to PAS. This may have to do with their deep seeded religious beliefs. Some surveys showed women as more opposed. A reason for this is because they are primarly care takers. They can see beyond the pain. However, patients with terminal illnesses had attitudes that were almost identical to the public. Physicians also has similar attitudes, however were less supportive if they were more likely to be called to actually perform the act. This may explain why oncologists (as many PAS patients have cancer) are the least supportive of physicians. (Emanuel, 2002)
According to a survey from Nashville-based LifeWay Research, even though millions of Americans disagree with assisted suicide, the majority (about two-thirds of the population) say that it should be morally acceptable for terminally ill patients to have access to physician assisted suicide. Suffering up until death should not be the only out. This survey can be seen in the figure below.
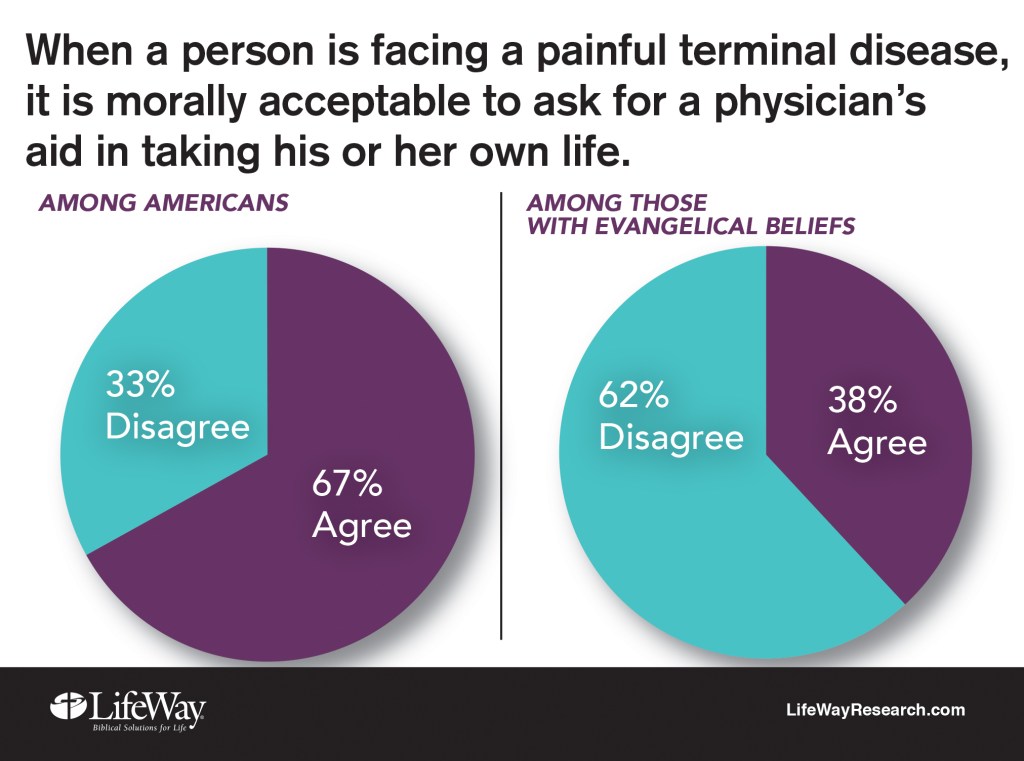
Most Americans Say Assisted Suicide is Morally Acceptable. (2017, August 23). Retrieved from https://lifewayresearch.com/2016/12/06/most-americans-say-assisted-suicide-is-morally-acceptable/
So far, the United States has not expanded the criteria past the terminally ill. An issue is including those who are suffering from mental health illness. Society still highly stigmatizes mental health and it is a topic that most of the public knows very little about. Furthermore, mental illness can manifest very differently in individuals, but we use umbrella terms to categorize a wide variety of mental health symptoms. Because most people are not well versed in the scope of mental illness it leaves us hesitant to expand the criteria of people eligible to choose PAS. This is the slippery slope that can lead to condoning a sort of holocaust. It, along with people with physical disabilities, was one of the first excuses that were used by physicians in the Nazi Party.
Another reason we have not expanded the criteria is not because we think that no one else could be suffering as much as patients who are terminally ill, but because citizens and policy makers may be fearful that expanding the criteria for PAS would mean we’d have to allow patients to choose to die when we have the technology to heal them and extend their lives.
There are three distinctions of euthanasia. The first is active and passive euthanasia. (Abohaimed, et. al, 2019) Which, while there is a very distinct legal line between active and passive euthanasia, sometimes making that decision to “let a person die” seems to be an active decision. This is can be seen in a Munson’s reading of Baby Owens from of a child with Down Syndrome and duodenal atresia that was asked to not be treated (Munson, 2008, pp 630-631). While this is technically passively letting the child die, making the decision to not treat an easily treatable case doesn’t feel passive. It seems that extending a life that has the potential to be long and happy should be done.
The second distinction of euthanasia is voluntary and nonvoluntary euthanasia. (Abohaimed, et. al, 2019) While we aren’t actively euthanizing people against their will (that would never be considered an allowable practice) there is talk about full consent regarding euthanasia. We want to use euthanasia to ease a person’s suffering, but not if they feel forced to do it because of social pressures. An article from Callahan talks about a person to have the ability to choose to be euthanized if the suffering is great and their autonomy needs to be respected when they make that decision (Munson, 2008, pp 706-711). The article does not address some of the social reasons an individual may feel forced to choose euthanasia. For example, “Dead at Noon” is a suicide note where Gillian Bennett felt that she was a burden and that her continued existence would increase the suffering of her family (Bennett, 2014). This letter can be read at the following link.
Social pressures can cause someone to pursue euthanasia and having the option may send the message to other people with similar cases that they are living lives that are not worth living. On the other hand, what one person deems as a good life may seem unbearable by another. While I agree that we need to be doing more to alleviate the social pressures that individuals like Bennett felt, I think that we will never be able to overcome all of them and that working on easing the lives of individuals suffering from diseases and disabilities can happen at the same time that euthanasia is being practiced. We cannot take away someone’s ability to make an autonomous decision because things “might” get better. And we cannot use future research or outcomes to justify actions that are taken in the moment.
The third distinction between euthanasia cases is speeding up a death verses ending a life. (Abohaimed, et. al, 2019) This is a harder distinction to make but is relevant when we are making policies in regard to euthanasia since most places require that you are terminally ill. An example of this would be for a baby who has a disease where its skin is falling off… people may want to be able to end the baby’s life despite it being an active killing because the baby was in constant pain and was terminally ill. On the other hand, Munson’s book includes a boy named Dax who is not allowed to die because he was not terminally ill even though he was in great pain (Munson, 208, 98-101). There seems to be a balance between autonomy and a terminal illness that is hard to strike. I believe that PSA and euthanasia is more than just about the fact of autonomy, but much more complicated. To adequately allow people with extreme suffering to choose PAS, the criteria for eligibility must be expanded.
One solution is that eligibility for PAS should be available to those who have maxed out their treatment options for mental and physical ailments. PAS is meant to decrease suffering in patients who really have no hope left. This is not adequately covered with only the terminally ill. If we were to expand the criteria to apply for PAS to include people who have maxed out the treatment options available for either their physical illness or their mental illness we could be more true to the reasons we have wanted PAS to be available for people. Maxing out treatment is not an easy thing to do and will take most people several years, but if there is truly no treatment available for a patient and they feel that they are in enough suffering to want to apply for PAS then we can confidently say as a society that there is not anything we could medically do to help them. This would not allow someone that has not maxed out treatment to choose PAS. It would exclude many illnesses such as those in the forms of depression which may happen even in our youth as there are many treatment options that work for those cases. Expanding eligibility for PAS to include those who have maxed out their treatment options will not cover all the cases of extreme suffering, but it is a step towards it and prevents a lot of the slippery slope arguments that prevent the policy from being expanded.
Another solution that has been used in the past is to allow PAS to terminally ill patients but require a waiting period of just in case people change their mind. PAS in the united states currently takes up to six weeks as you need to go through the court process, see a psychiatrist, and have two physicians sign off on it before you are prescribed the lethal dose of medication. This makes it go over better in our society but adds a lot of unnecessary time for the patient that has made the decision already.
Another solution is not to allow PAS at all, but to have adequate pain control even at the risk of hastening a patient’s death. This allows a physician to still follow the five principles of bioethics as their intention is still to help their patient alleviate pain.
Another solution is for the patient to just commit suicide unassisted by the physician. Suicide is within the means of most people. I think that it is a choice that people must make. If you think that it’s going to be painful, then you lack imagination. I don’t believe it’s a moral choice to make, but it’s not my place to judge. I just don’t think you should put another person in that position.
I think that dying naturally teaches lessons. It teaches grace and is a time for communication that people can wrap up their lives and forgive or be forgiven. It is connected with our birth as I believe life is a circle and if you interrupt that circle you lose some of the essence of life. If you miss that time period, you miss one of the major life events that make us human. The debate over physician-assisted suicide is unlikely to go away and it raises troublesome questions. It requires continuous ethical monitoring because it allows a person to start justifying the taking of a life.
Bibliography
Abohaimed, S., Matar, B., Al-Shimali, H., Al-Thalji, K., Al-Othman, O., Zurba, Y., & Shah, N. (2019). Attitudes of Physicians towards Different Types of Euthanasia in Kuwait. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6598031/
Bennett, Gillian. (2014) Dead at Noon. Retrieved from http://www.deadatnoon.com/. Website.
Charlotte Lozier Institute. (n.d.). Map: Assisted Suicide in the States. Retrieved from https://lozierinstitute.org/map-assisted-suicide-in-the-states/
Emanuel, E. J. (2002, January 28). Euthanasia and Physician-Assisted Suicide. Retrieved from https://jamanetwork.com/journals/jamainternalmedicine/article-abstract/214736
Guy, M., & Stern, T. A. (2006). The desire for death in the setting of terminal illness: a case discussion. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1764532/
Jr., W. C. S. (2018, March 6). Medical Definition of Hippocratic Oath. Retrieved from https://www.medicinenet.com/script/main/art.asp?articlekey=20909
Most Americans Say Assisted Suicide is Morally Acceptable. (2017, August 23). Retrieved from https://lifewayresearch.com/2016/12/06/most-americans-say-assisted-suicide-is-morally-acceptable/ Munson, Ronald. (2008) Intervention and Reflection: Basic Issues in Medical Ethics. 8th edition. Thomson Higher Education; Belmont, CA. pp 630-631 and 98-101. Print.
Physician Assisted Suicide. (n.d.). Retrieved from https://illinoisrighttolife.org/physician-assisted-suicide/